WATERFALL Trial
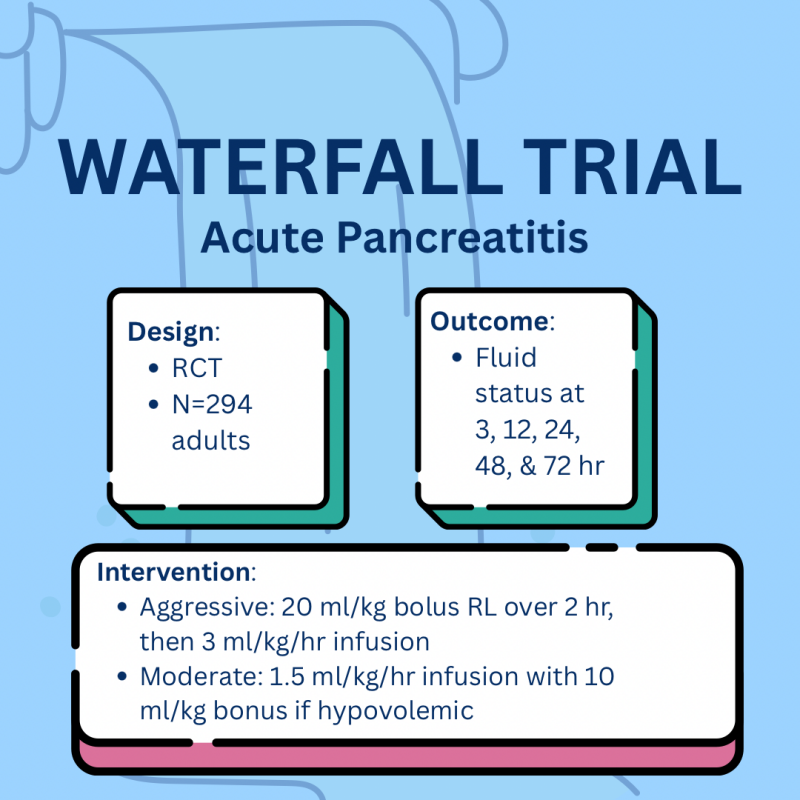
This multicenter RCT (N=294) asked a key question: Does aggressive fluid resuscitation improve outcomes in acute pancreatitis compared to moderate resuscitation?
🧪 Intervention
Aggressive: 20 mL/kg bolus over 2 hrs + 3 mL/kg/hr infusion
Moderate: 1.5 mL/kg/hr + 10 mL/kg bolus if hypovolemic
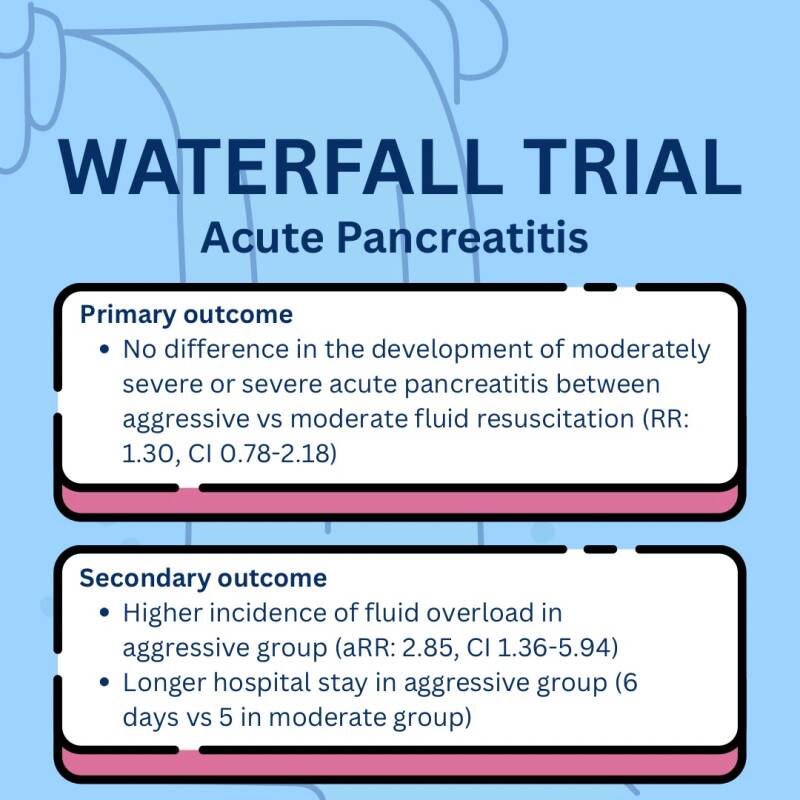
📌 Primary Outcome:
No difference in progression to moderately severe/severe pancreatitis (RR: 1.30, CI 0.78–2.18)
📌 Secondary Outcomes:
- ↑ Fluid overload in aggressive group (aRR 2.85)
- Longer hospital stay (6 vs 5 days)
🔚 Conclusion:
More fluid ≠ better outcomes. Aggressive hydration led to more harm (fluid overload) without benefit.
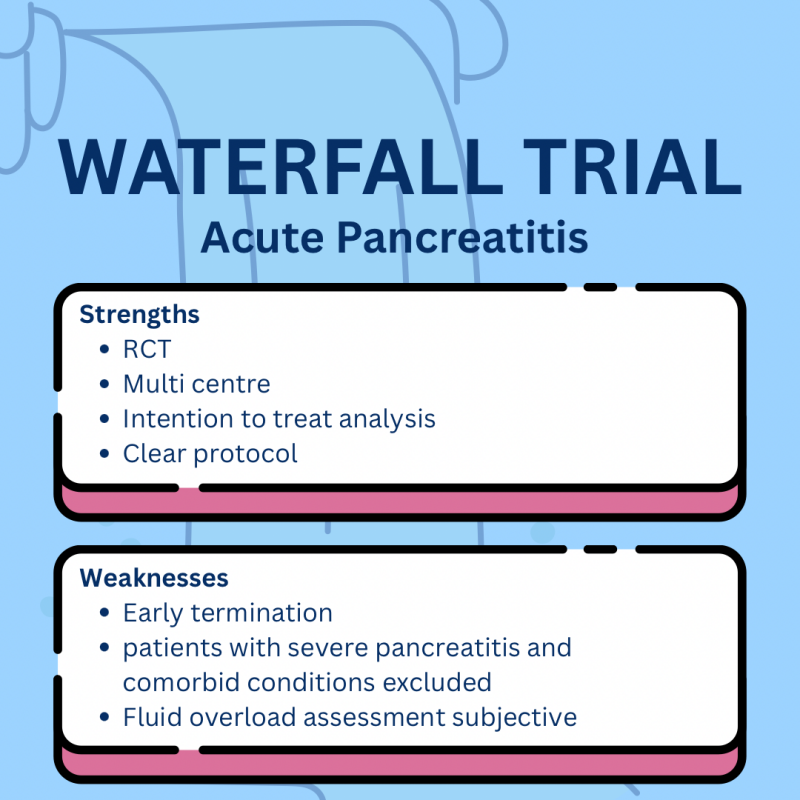
✅ Strengths: RCT, clear protocol, ITT analysis
⚠️ Limitations: Early termination, exclusion of severe cases, subjective fluid overload assessment
SPRINT Trial
This landmark NEJM trial aimed to determine whether targeting a lower systolic blood pressure (SBP) <120 mm Hg reduces cardiovascular events and mortality compared to a standard target of <140 mm Hg in patients without diabetes but at high cardiovascular risk.
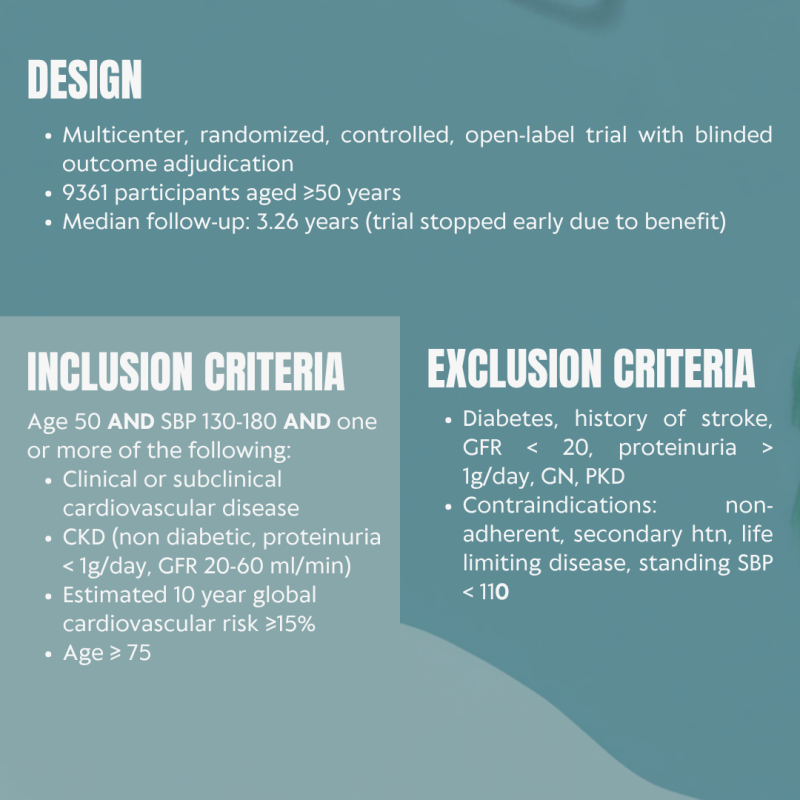
🧪 Design:
RCT with 9,361 patients aged ≥50 years, high CV risk, no diabetes, no history of stroke
💊 Intervention:
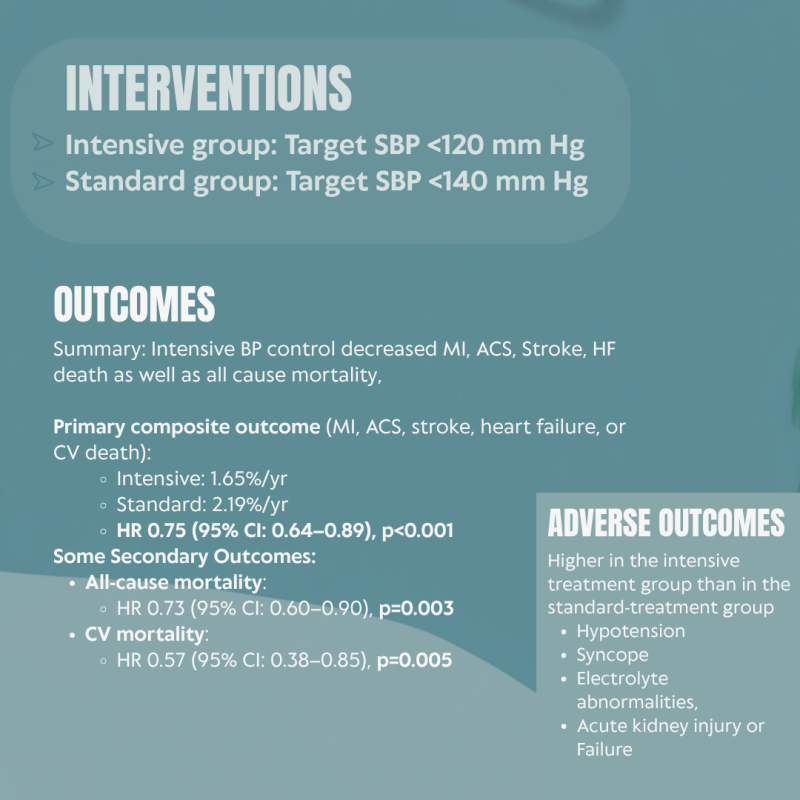
🔹 Intensive BP control (<120 mmHg)
🔹 Standard BP control (<140 mmHg)
📉 Adverse outcomes: Hypotension, Syncope, Electrolyte abnormalities, Acute kidney injury
🎯 Outcome: Intensive SBP control (<120 mmHg) decreased MI, ACS, Stroke, HF death as well as all-cause mortality and CV mortality
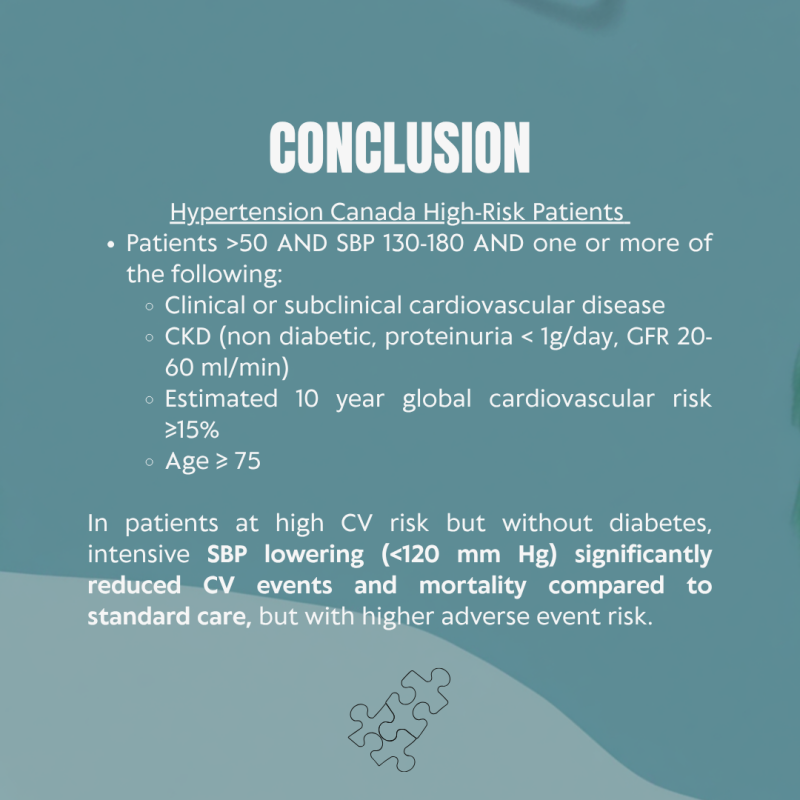
Conclusion:
✅ This study supports more aggressive BP targets in selected high-risk populations.
✅ In patients at high CV risk but without diabetes, intensive SBP lowering (<120 mm Hg) significantly reduced CV events and mortality compared to standard care, but with higher adverse event risk.

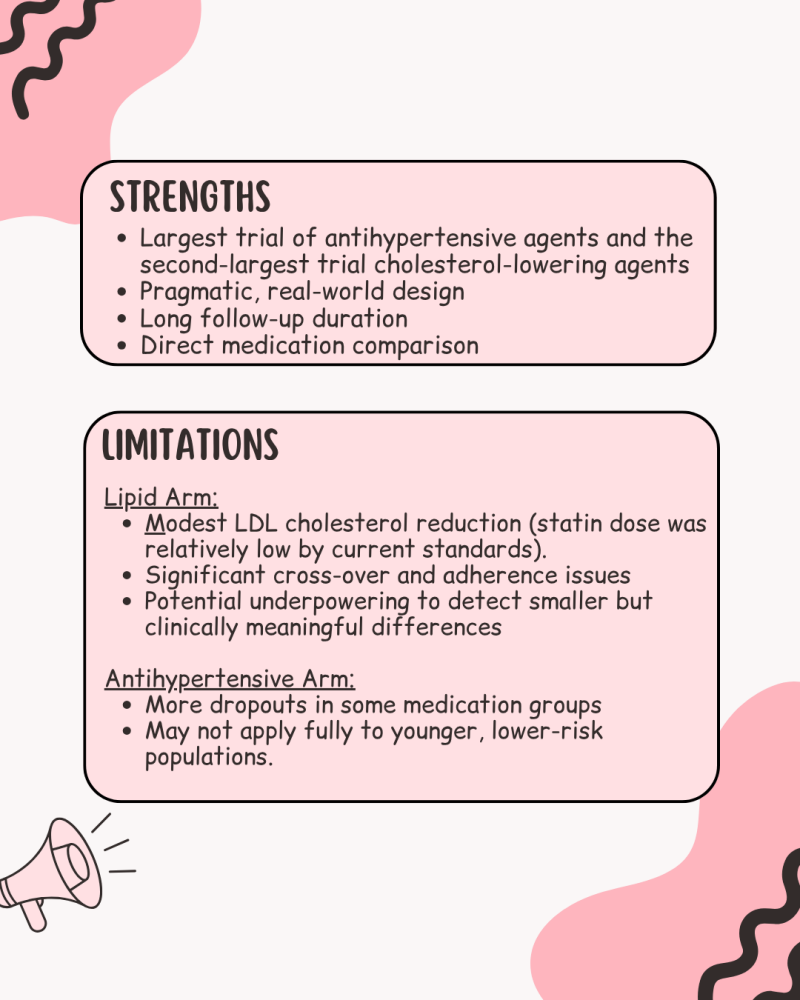
ALLHAT Trial
💊 Objective: To compare CV outcomes across anti-hypertensive drug classes and assess the impact of pravastatin on mortality and coronary events in hypertensive patients
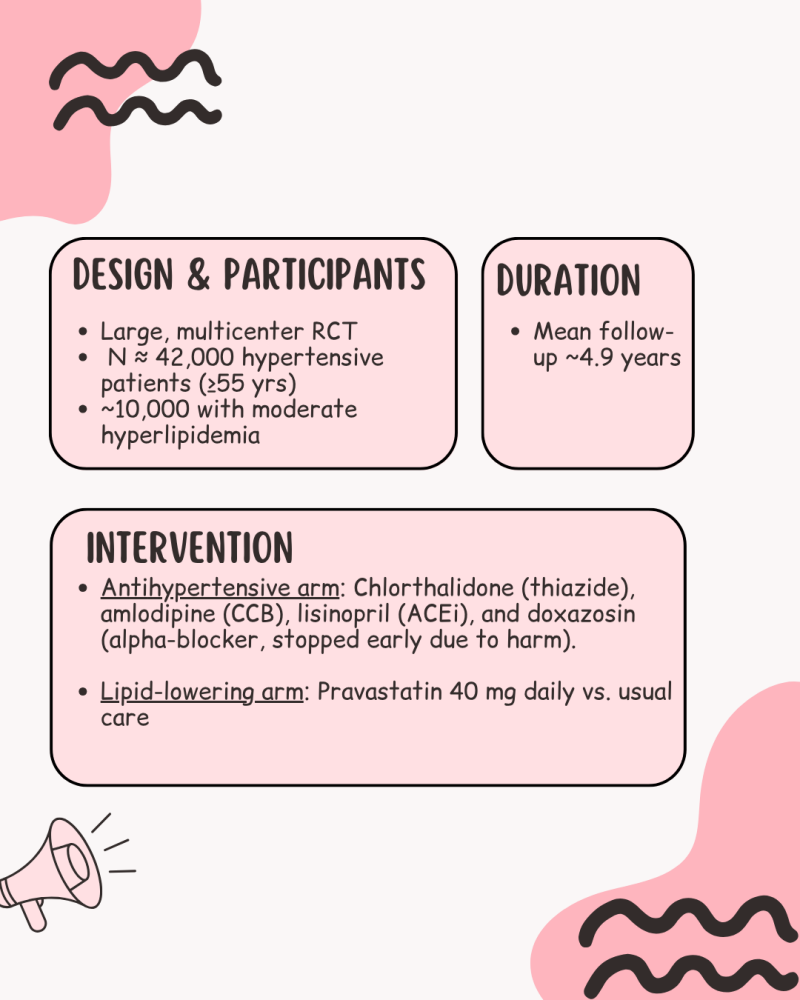
Methods
👥 42,000+ patients with HTN
🧪 Compared:
• Anti-hypertensive arm: Thiazide vs CCB vs ACEi
• Lipid-lowering arm: Pravastatin vs usual care
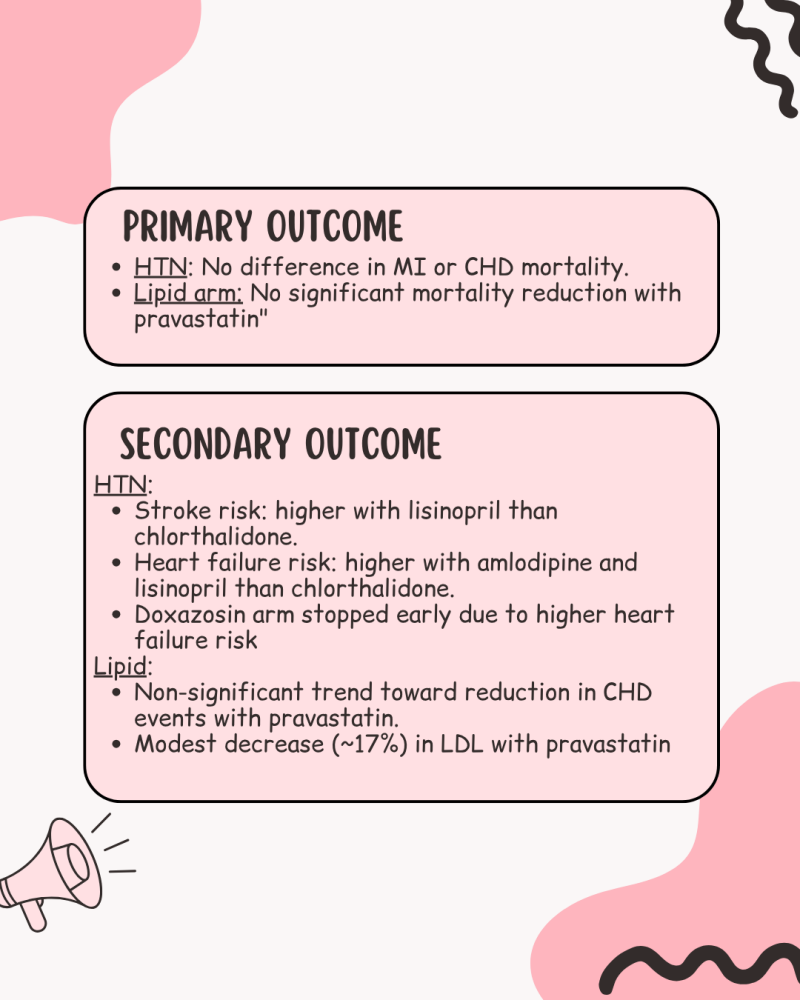
📌 Key Takeaways:
• Anti-hypertensive arm: No major difference in MI or CHD mortality between antihypertensives
• Lipid-lowering arm: No significant mortality reduction with pravastatin
📈 Secondary Outcomes
• Chlorthalidone outperformed others on stroke and heart failure risk
• ACEi and CCB had higher heart failure rates
• Statin arm showed only modest LDL reductions (~17%) and no significant outcome benefit
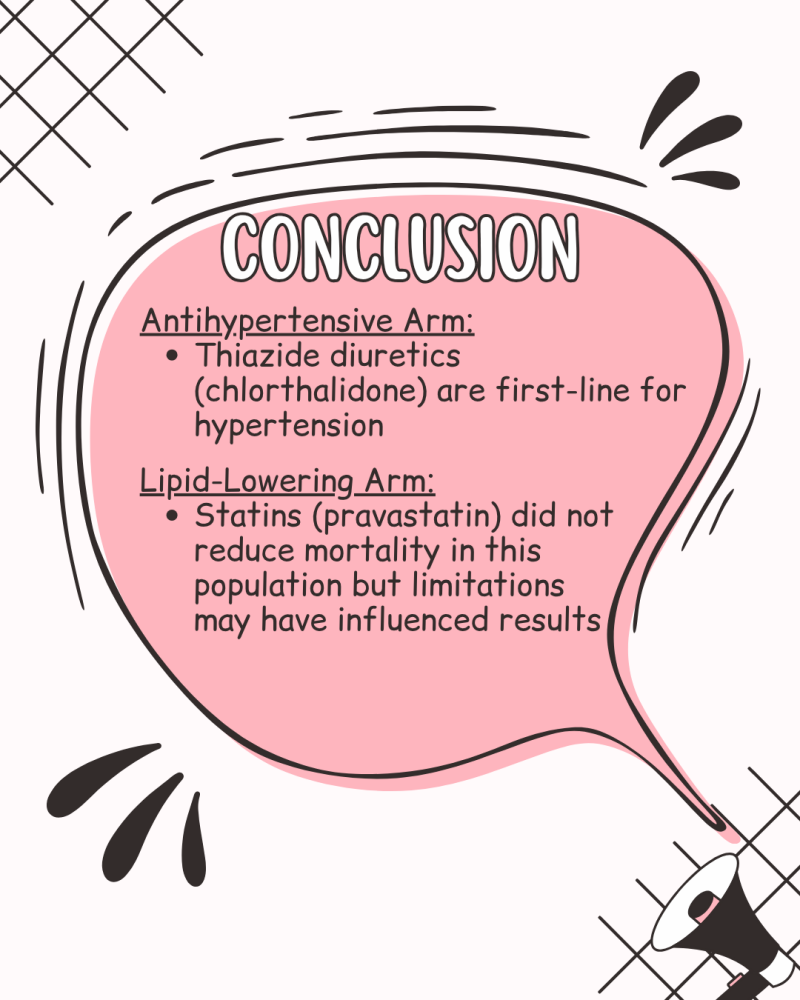
📚 Conclusion:
• Thiazide diuretics are your go-to first-line for uncomplicated hypertension
• Statins may need higher doses or better adherence to show benefit in certain populations
ACCORD Trial
🎯 Objective:
Does intensive control of blood glucose, blood pressure, and lipids reduce CV events in high-risk patients with T2DM?
🧪 Design:
Multicenter, randomized controlled trial
👥 10,251 patients with type 2 diabetes at high cardiovascular (CV) risk
📌 Trial Arms & Targets:
🔵 Glycemic Control: A1c <6.0% vs. standard 7.0–7.9%
🔵 Blood Pressure Control: SBP <120 mmHg vs. <140 mmHg
🔵 Lipid Control: Fenofibrate + statin vs. statin alone
📉 Primary Outcomes:
❌ Glycemic Arm: No reduction in major CV events. Increased mortality → arm stopped early
❌ BP Arm: No significant CV benefit. Lower stroke risk (secondary finding) but more side effects
❌ Lipid Arm: No added benefit from fenofibrate when added to statin therapy
🔍 Conclusion:
⚠️ More intensive treatment did not reduce CV events
✔️ Intensive glycemic control increases mortality risk and does not reduce CV events in high risk patients with T2DM
✔️ BP control <120 mmHg may lower stroke risk but does not reduce major CV events
✔️ Statins remain the foundation of lipid management, as adding fibrates do not add CV benefit
💪 Strengths:
- Large, diverse high-risk population
- Comprehensive assessment of 3 major CV risk factors
- Robust RCT design across multiple centers
⚠️ Limitations:
- Glycemic arm stopped early → less long-term data
- Increased adverse events (hypoglycemia, hypotension)
- Findings may not generalize to younger/lower-risk patients
- BP arm may have been underpowered







Create Your Own Website With Webador